What is the cornea?
The cornea is a clear, dome-shaped surface that makes up the outermost layer of the eye. Because it contains no blood vessels, it must receive nourishment from tears and the aqueous humor, a fluid that lies just behind the cornea.
The cornea is composed of five unique layers:
- The Epithelium– Thin and nerve-filled, this is the outermost layer of the cornea. It blocks the passage of foreign substances and aids in the absorption of oxygen and nutrients from tears.
- Bowman’s Membrane – This second layer is composed of collagen. This layer can heal if injured, although large or centrally-located scars can cause vision loss.
- Stroma– The third and thickest layer of the cornea is primarily composed of collagen and water. Its unique characteristics allows for light to be conducted while maintaining strength, elasticity and form.
- Descemet’s Membrane – This thin, strong film provides protection against infection or injury. It is made primarily of collagen and is easily repaired after injury
- Endothelium– This thin, innermost layer keeps the cornea clear. This layer is responsible for pumping fluid out of the stroma. Endothelial cells do not regenerate, and cannot be repaired or replaced by the body.
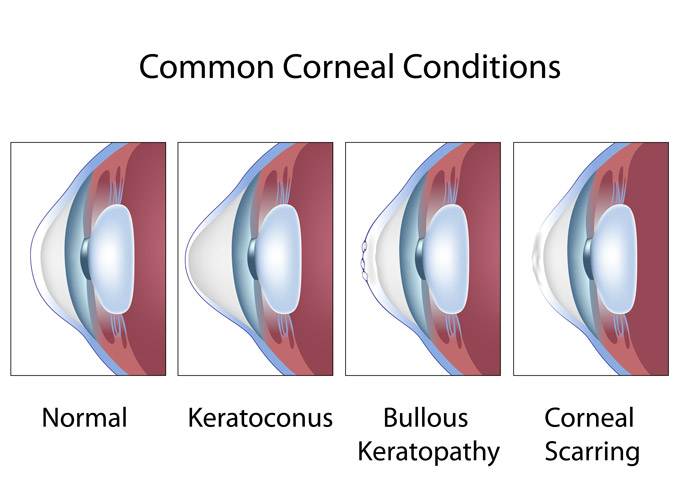
Which conditions affect the cornea?
Multiple diseases, disorders, and injuries can impact the cornea. It is important to select an ophthalmologist who is knowledgeable and experienced in detecting and treating corneal problems early to prevent long-term eye problems.
Corneal conditions include:
- Keratoconus
Keratoconus is a progressive illness in which the cornea gradually thins and bulges into a cone-like shape. Because of this, the cornea is distorts light as it enters the eye, resulting in nearsightedness and irregular astigmatism.
Symptoms of keratoconus include:
- Blurred vision
- Glare and halos at night
- Increased sensitivity to light
- Frequent prescription changes
Keratoconus can be treated with special contact lenses or surgery.
- Bullous Keratopathy
Bullous keratopathy is an eye condition characterized by a blister-like swelling of the cornea. This condition is most common in older adults and may be a rare complication of cataract surgery.
Symptoms of bullous keratopathy include:
- Fluid-filled blisters on the cornea
- Increased sensitivity to light
- Blurred vision
- Feeling like there’s a foreign object trapped in the eye
Bullous keratopathy can be treated with eye drops, soft contact lenses, and drugs designed to lower eye pressure. In rare cases, patients may require a corneal transplant.
- Fuchs’ dystrophy
Fuchs’ dystrophy is a progressive disease in which cells in the corneal endothelium gradually break down, resulting in vision problems. This disease is more common in women than men, and is more common in older adults.
Symptoms of Fuchs’ dystrophy include:
- Difficulty seeing at night
- Blurred vision in the morning that gradually improves during the day
- Painful blisters on the cornea
- Increased light sensitivity
- Cloudy cornea
Drops, ointments, and soft contact lenses can help reduce the swelling associated with the disease. In some cases, a corneal transplant might be necessary.
What is a corneal transplant?
A corneal transplant, also known as keratoplasty, is performed when a patient’s cornea no longer allows light to enter the eye properly due to injury or disease. The goal of this procedure is to restore vision loss caused by the damaged cornea.
During this procedure, an eye surgeon removes part of your cornea and replaces it with corneal tissue provided by a donor. In some instances, a surgeon may elect to transplant a small portion if the disease or damage is limited to a small portion of the cornea.
Healing time, success rates, and risks associated with corneal transplants vary based on the type of transplant. It is important to select an experienced eye surgeon who can recommend the best treatment options and long-term care options available to you.
For more information about corneal conditions – as well as treatment method – contact South East Eye Clinic today.






